GNTI-122, an autologous engineered Tregs product designed to treat type 1 diabetes.
GNTI-122
GNTI-122 is an autologous engineered Tregs (EngTregs™) product designed to protect beta cells from destruction by the immune system. GNTI-122 is being developed for the treatment of patients who are newly diagnosed with or at high risk for developing T1D, a progressive autoimmune disease, by restoring the body’s normal immune tolerance to pancreatic islets. GNTI-122 also leverages the unique properties of EngTregs to promote an environment that will support repair and improve function of inflamed and damaged beta cells.
GNTI-122 is engineered to express a pancreatic islet-specific T cell receptor (TCR) to target the engineered Tregs to the site of disease together with modifications to stabilize and increase expression of the FOXP3 protein and the insertion of a chimeric IL-2 signaling complex, which provides GentiBio’s EngTregs with exclusive proliferative and functional support. GNTI-122 is designed to be a highly selective, potent, and durable immune modulatory therapy that is tunable after administration.
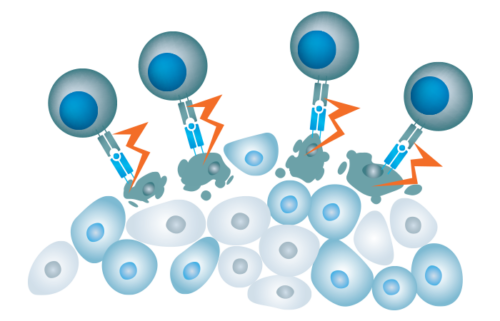
In T1D, effector T cells lose their tolerance for self-antigens expressed on pancreatic beta cells and bind to and destroy these cells
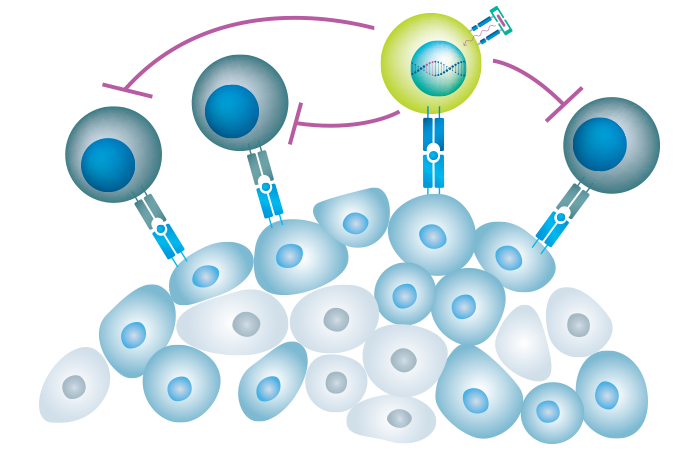
GNTI-122 protects islet cells from damage by homing to the pancreas and draining lymph nodes and suppressing pathogenic effector T cells via the mechanisms of bystander suppression and infectious tolerance
About Type 1 Diabetes
Type 1 Diabetes (T1D) is a serious autoimmune disease caused by T cell-mediated destruction of insulin producing beta cells in the pancreas. This beta cell loss ultimately results in uncontrolled hyperglycemia and life-long dependence on daily insulin administration. The daily demands of glucose monitoring and insulin administration are challenging for T1D patients, undermining patients’ quality of life. Current insulin replacement options are insufficient to replicate normal glycemic control, and for this reason, T1D is also associated with debilitating and life-threatening outcomes such as diabetic ketoacidosis, hypoglycemic events and micro- and macrovascular complications such as ischemic heart disease, strokes, retinopathy, and nephropathy. Disease modifying therapies that can prevent or delay beta cell loss and maintain normal glucose control are urgently needed.

